When your Child Can’t Breathe
by Hatzalah of Baltimore
“It was 2 a.m. I
woke up to a barking noise and ran to my child’s room, where I found my three-year-old
awake and having trouble breathing. She had had a cold for a few days, but this
was new. I took her into the bathroom and ran the hot water from the shower to
make steam. That seemed to help a little. I was hesitant to call Hatzalah in
the middle of the night, but I was really worried and decided to go ahead. Two
guys arrived within minutes and started treatment.”
* * *
This case from
Hatzalah’s files is just one of many similar ones. In fact, pediatric breathing
difficulties are among the most common pediatric medical emergencies. The
airways of babies and children are smaller and narrower than adult airways, and
their tongues are larger, making it easy to obstruct their airways, resulting
in difficulty breathing. A variety of respiratory medical conditions affect one
or more areas of the air passages, causing breathing difficulties.
Infection is the
most common cause of breathing problems in children, and it is usually caused
by a virus. The common cold, croup, respiratory syncytial virus (RSV),
influenza, bronchitis, and bronchiolitis are generally viral conditions. These are
frequently treatable at home, but it is critical for parents to understand the “breathing”
or respiratory process so as to recognize when an ambulance or emergency room
is required.
Nasal congestion
from the common cold is common, but the same common cold causing virus can be
worse, as with RSV, which affects the upper and lower airways. In croup the
upper airway in the neck narrows due to inflammation. The child makes a
whistling sound while breathing through the constricted airway. Sometimes, there
is a cough that sounds like a “barking” seal.
Other medical
issues that may affect breathing include asthma, foreign body airway
obstruction, allergic reactions, neurological, and heart and lung disorders.
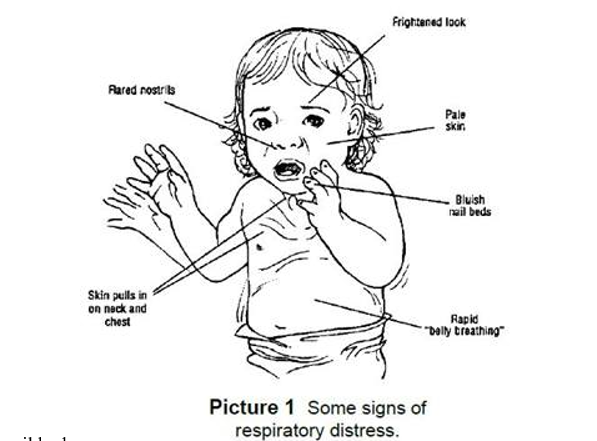
When a person is struggling to breathe, they are said to be in respiratory distress. You may notice
different symptoms depending on where the illness is located in the respiratory
system.
The purpose of
this article is to address common respiratory emergencies and educate parents
as to when to call for help.
When Should a Parent Become Concerned?
If your child is
ill, contact your healthcare provider for advice and assistance. Treatment is
generally supportive, which means treating fever with a non-aspirin anti-fever
medication, such as acetaminophen (Tylenol), using a cool mist humidifier, and
blowing or clearing nostrils with a bulb syringe. They most likely do not
require an ambulance or a trip to the emergency room. However, any infant with
a fever who is less than two months old needs to be evaluated.
If you see any of
the following symptoms, however, you should call Hatzalah. If in doubt, do not
worry about looking foolish. Just call.
•
Breathing rate: A child may be having trouble
breathing or not getting enough oxygen if their number of breaths per minute
increases. If a baby under one year old is breathing more than 60 times per
minute, or if a child over one year old is breathing more than 40 times per
minute, the breathing rate is too fast.
•
Low oxygen level: Oxygen levels can
be checked with a pulse oximeter, a small, fingertip device that costs 15 to 20
dollars. Oxygen levels should be higher than 92%.
•
Color changes: A child may have a bluish hue
around the mouth, on the inside of their lips, or even on their fingernails if
they are not obtaining enough oxygen. The skin may also seem pale or gray.
•
Grunting: With each exhalation, the child may make a
grunting noise. This is an effort to keep the lungs filled with air and keep
them open.
•
Nasal flaring: A child may be breathing more
laboriously if their nose apertures widen apart while they breathe.
•
Retractions: With each breath,
the chest seems to pull in on the lower neck, the chest, and/or under the
breastbone, which is an attempt to fill the lungs with more air.
•
Wheezing and stridor: Noisy breathing
may be a sign of an emergency if the child appears to be having respiratory
distress.
•
Accessory muscle use: When your child
breathes in, it appears as though the muscles in the neck are moving. This can
also be visible in the muscles between the ribs or underneath the rib cage.
Rapid belly breathing is also a concern.
•
Changes in alertness and appearance: Your child’s
excessive tiredness could be a sign of low oxygen levels and could also point
to respiratory exhaustion. Children should not appear anxious or frightened.
•
Body positions: Your child may
thrust his or her head backwards while having difficulty breathing due to low
oxygen levels (especially if lying down). Alternatively, while seated, your
child might lean forward. When everything else fails, children will naturally
use these positions to help their respiration.
If you notice any
of these symptoms call Hatzalah immediately at 410-358-0000.
It is important to
prevent the spread of infection by keeping ill children away from well children,
practicing good hand washing, and making sure that your child’s immunizations
are up to date.






